Revision Shoulder Replacement
Replacement
Revision Shoulder Replacement
Grasping the essence of life involves everyday tasks like combing your hair, getting dressed, lugging groceries, and enjoying uninterrupted sleep. Yet, accomplishing these simple tasks can become challenging when shoulder mobility is limited. Fortunately, there are various treatments available for shoulder pain, with shoulder replacement surgery being one option.
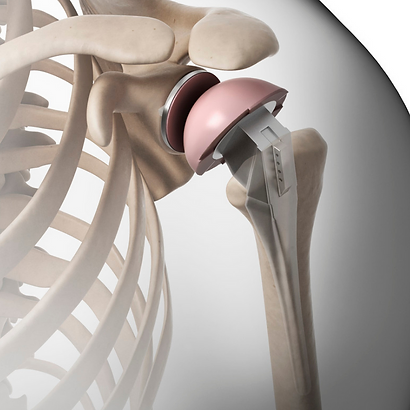
The shoulder constitutes a ball and socket joint primarily composed of two bones: the upper arm bone (humerus) housing the ball portion, and the shoulder blade housing the socket portion. This arrangement allows for the fluid movement of the shoulder.
Smooth cartilage, akin to rubber, covers the ball and socket, serving as a cushioning layer. This cartilage ensures smooth movement between the bones, preventing friction or damage to their surfaces.
Three common conditions that damage the cartilage
Wear and tear osteoarthritis begins when the cartilage, which cushions the joints, is damaged or worn away. This leads to the bones rubbing against each other, causing pain. Over time, this friction wears down the surfaces of the bones. Unfortunately, there’s no medication or treatment available to regenerate damaged cartilage.
A Proximal humerus fracture, simply put, is a broken shoulder. It occurs when the upper arm bone breaks at the shoulder joint. This type of injury is common among older individuals with osteoporosis, where bones become more fragile and prone to fractures from falls or impacts, like those from car accidents.
Rotator cuff arthropathy develops when the tendons stabilizing the shoulder, known as the rotator cuff, tear, increasing stress on the joints and leading to cartilage damage.
Shoulder joint replacement is a complex surgical procedure. While total shoulder arthroplasty (TSA) is generally successful, a subset of these surgeries may fail and require revision. Revision surgery is often necessary due to issues such as loosening of the implant, rotator cuff tears, infection, or instability. The success of revision surgery, whether switching to another type of joint replacement or not, can vary depending on the cause for revision and the type of implant used.
Common causes of shoulder arthroplasty failure
Prior to undertaking a surgical revision of a shoulder arthroplasty, it’s crucial to ascertain the underlying issues faced by the patient. The subsequent enumeration outlines the prevalent causes of failure in shoulder arthroplasty:
- Infection
- Reactivity to polyethylene or polymethylmethacrylate
- Fracture
- Stiffness
- Inadequate rehabilitation
- Presence of unwanted bone
- Tuberosity malunion
- Overstuffing of the joint
- Instability
- Anterior instability
- Subscapularis deficiency
- Glenoid component anteversion
- Tuberosity nonunion
- Supraspinatus/infraspinatus defect
- Humeral component anteversion or anterior head offset
- Insufficient anterior glenoid bone
- Posterior instability
- Glenoid component retroversion
- Posterior cuff defect
- Excessive humeral component retroversion or posterior head offset
- Insufficient posterior glenoid bone
- Superior instability
- Loss of rotator cuff
- Loss of the coracoacromial arch
- Weakness
- Reduced muscle strength
- Subscapularis deficiency
- Supraspinatus/infraspinatus deficiency
- Tuberosity nonunion or malunion
- Deltoid detachment
- Nerve injury
- Malpositioned humeral component
- Loose humeral component
- Eroded glenoid bone (hemiarthroplasty)
- Malpositioned glenoid component
- Loose glenoid component
Preparing for Revision Surgery
The patient's medical history and past records are carefully assessed to understand their shoulder condition before the primary arthroplasty procedure. Details regarding the reconstruction, such as the brand, model, and size of the prostheses used, are examined. Additionally, the rehabilitation process is investigated, along with any signs of infection, allergic reactions, or recent injuries. The patient's overall health status, including factors like nutrition, pain levels, medication usage, smoking and alcohol habits, and other concurrent medical conditions, are also considered.
A thorough examination of the shoulder's range of motion, stability, strength, and smoothness is conducted. Diagnostic tests such as electromyography (EMG), nerve conduction studies, computed tomography (CT) scans, and specialized sonography may be employed to assess nerve function, bone integrity, and the condition of the rotator cuff.
Laboratory investigations typically include a complete blood count (CBC), sedimentation rate analysis, and serum albumin level assessment. Radiographic imaging comprises an anteroposterior view in the scapular plane, an axillary view, and a full-length humeral view to comprehensively evaluate the shoulder joint.
