Bankart’s/Labrum Repair
Arthroscopy
Bankart Lesion/Labrum Repair
One of the key components of the shoulder is its ball-and-socket configuration, facilitating arm rotation. In a healthy shoulder, the ball (known as the humeral head) sits centered within the shallow socket (the glenoid or glenoid cavity), maintaining stability.
Adding to this stability is the glenoid labrum, a fibrocartilaginous rim encircling the edge of the glenoid, deepening its concavity. Various ligaments, some connected to the glenoid labrum, assist in keeping the humeral head within its socket. Collectively, these bones and tissues ensure the shoulder remains stable during a wide range of motion.
However, sudden shoulder trauma or repetitive strain can cause a forceful dislocation, resulting in the tearing of the shoulder’s cartilage and ligaments, particularly below the center anterior (front) of the socket, known as a Bankart lesion. This tear compromises the labrum, allowing the humeral head to displace farther than normal.
Most Bankart lesions occur due to anterior dislocations, wherein the arm moves excessively forward and downward, often during side-arm extension. Posterior dislocations (forced backward movement of the arm) can also cause labral tears, albeit less frequently.
Should a fracture accompany the tear in the shoulder blade (scapula) or shoulder socket (glenoid cavity), it is termed a bony or osseous Bankart lesion.
If left untreated, a Bankart lesion can lead to chronic shoulder instability, predisposing the shoulder to future dislocations, even with lesser force than the initial injury.


Causes
Bankart lesions often stem from various incidents such as collisions, accidents, and sports-related injuries, whether they are acute impacts or strains from repetitive arm movements. Although anyone can experience this type of injury, it’s most commonly observed in young men in their twenties.
Factors contributing to shoulder dislocations and lesions include:
Car Accidents: A sudden impact on the shoulder can dislodge the ball from its socket, resulting in labrum tears.
Sports Collisions: High-speed collisions with another person, as seen in sports like football or hockey, can forcefully push the shoulder out of alignment or pull the arm forward or backward, leading to dislocations.
Sports Falls: Athletes falling and landing on their shoulders, particularly prevalent in sports involving heights or speed such as gymnastics, skating, rollerblading, or skiing, can cause shoulder dislocations.
Non-Sports Falls: Falling from heights such as a ladder or tripping on uneven surfaces can exert sufficient force to dislocate the shoulder. Older adults and individuals with walking difficulties are particularly vulnerable to such accidents.
Overuse Injuries: Some athletes may develop loose ligaments and instability in the shoulder due to repetitive strain. This is common among swimmers, tennis players, volleyball players, baseball pitchers, gymnasts, weightlifters, and even non-athletes engaged in activities involving repetitive overhead arm motions, like swinging a hammer.
Genetic Predisposition: Certain individuals may inherit a tendency for loose ligaments throughout their body, making their shoulders prone to easy misalignment, especially in double-jointed individuals.
Physical Abuse: Instances of domestic violence, bullying, or fighting can involve falls, blows, or sudden movements that forcefully dislocate the shoulder and cause damage to surrounding tissues.
Symptoms
Symptoms of a shoulder issue may include :
Pain: Experienced when performing overhead activities such as throwing a ball or combing hair.
Instability and weakness: The shoulder might feel as though it's hanging loosely, dislocating easily, or lacking strength.
Limited range of motion: Difficulty moving the shoulder suddenly in any direction could suggest a tear.
Unusual sensations or noises in the shoulder.
Grinding, catching (motion feels non-fluid), locking, or popping sensations, which may indicate torn tissue catching within the joint.
Treatment
Non-Surgical
For older patients or individuals with limited activity levels, it is advisable to pursue non-surgical options for addressing a Bankart lesion. Initially, the affected arm is placed in a sling for several weeks, typically positioned across the front of the body with internal rotation (inward turning), and supported by a small pillow under the armpit to keep it slightly away from the body. Subsequently, intensive physical therapy is undertaken to restore strength, stability, and mobility to the shoulder. However, a drawback of this treatment approach is that the glenoid labrum, while in this resting position, may heal slightly out of alignment, reducing the depth of the socket and increasing the likelihood of recurrent dislocations.
Surgical
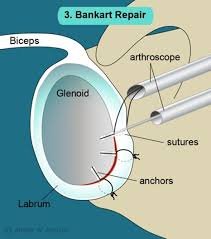
Bankart repair surgery is typically the preferred treatment for younger patients with a Bankart lesion, particularly those engaged in sports, as they face a heightened risk of recurring shoulder dislocations. This is due to the common inadequacy of the glenoid labrum tear to fully heal, resulting in insufficient socket depth, thus reducing stability and elevating the likelihood of further dislocation. The procedure for repairing a Bankart lesion is usually conducted arthroscopically (using keyhole surgery) under general anesthesia. The objective of this surgery is to mend and tighten stretched and damaged ligaments, joint capsule, and cartilage. Suture anchors are embedded in the bone, securing the torn glenoid labrum back to the glenoid fossa. Typically, patients can return home the same day or the following day after undergoing Bankart repair. During the initial weeks following surgery, it is necessary to wear a sling, even during sleep, to shield the shoulder and promote healing in the correct alignment. Physical therapy begins shortly after the procedure to rebuild strength, enhance stability, and regain mobility. Patients are provided with a rehabilitation program to adhere to, gradually advancing to more demanding exercises over time. Full recovery from Bankart repair and a return to contact sports usually take around 4-6 months.
